Background and purpose of the study
Migraine
headache is a common and potentially debilitating disorder often treated by
family physicians. Before diagnosing migraine, serious intracranial pathology
must be ruled out. Treating acute migraine is challenging because of
substantial rates of nonresponse to medications and difficulty in predicting
individual response to a specific agent or dose. Data comparing different drug
classes are relatively scarce. Abortive therapy should be used as early as
possible after the onset of symptoms. Effective first-line therapies for mild
to moderate migraine are nonprescription nonsteroidal anti-inflammatory drugs
and combination analgesics containing acetaminophen, aspirin, and caffeine.
Triptans are first-line therapies for moderate to severe migraine, or mild to
moderate migraine that has not responded to adequate doses of simple
analgesics. Triptans should be avoided in patients with vascular disease,
uncontrolled hypertension, or hemiplegic migraine. Intravenous antiemetics,
with or without intravenous dihydroergotamine, are effective therapies in an
emergency department setting. Dexamethasone may be a useful adjunct to standard
therapy in preventing short-term headache recurrence. Intranasal lidocaine may
also have a role in relief of acute migraine. Isometheptene-containing
compounds and intranasal dihydroergotamine are also reasonable therapeutic
options. Medications containing opiates or barbiturates should be avoided for
acute migraine. During pregnancy, migraine may be treated with acetaminophen or
nonsteroidal anti-inflammatory drugs (prior to third trimester), or opiates in
refractory cases. Acetaminophen, ibuprofen, intranasal sumatriptan, and
intranasal zolmitriptan seem to be effective in children and adolescents,
although data in these age groups are limited. (Am Fam Physician. 2011;83(3):271-280. Copyright © 2011 American Academy
of Family Physicians)
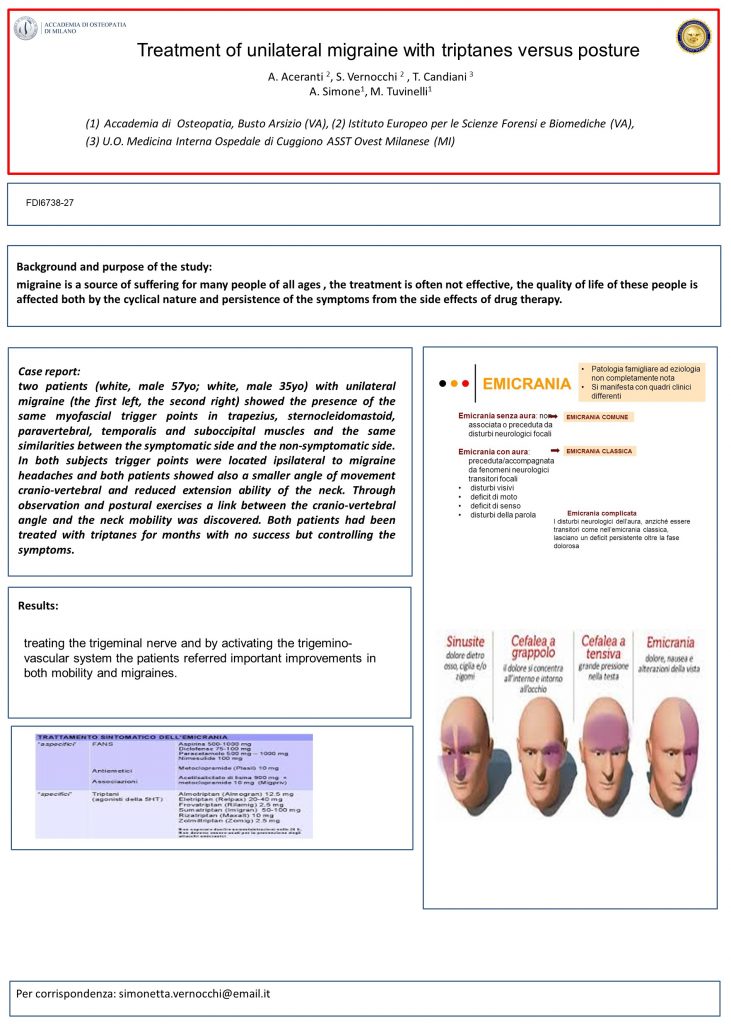
Triptans
are migraine-specific drugs that bind to serotonergic receptors. They are
considered first-line therapy for moderate to severe migraine, or mild to
moderate attacks unresponsive to nonspecific analgesics. Seven triptans are
currently available, but data guiding which to select for an individual patient
are limited. A Cochrane review found that all triptans are similar in effectiveness
and tolerability. A meta-analysis of 53 trials using oral triptans found that
the three most effective agents for pain relief were 10 mg of rizatriptan
(Maxalt), 80 mg of eletriptan (Relpax), and 12.5 mg of almotriptan (Ferrari MD, Roon KI, Lipton RB, Goadsby PJ.
Oral triptans (serotonin 5-HT(1B/1D) agonists) in acute migraine treatment: a
meta-analysis of 53 trials. Lancet. 2001;358(9294):1668-1675). A Cochrane
review found a dose of 100 mg of sumatriptan to be more effective than lower
doses (McCrory DC, Gray RN. Oral
sumatriptan for acute migraine. Cochrane Database Syst Rev. 2003;(3):CD002915).
It is sometimes necessary to increase the dose of an individual agent before
judging response. Trials suggest that nonresponders to one triptan may respond
to another; therefore, switching triptans is also reasonable. Triptans differ
from one another in pharmacokinetics. Rizatriptan has a quicker onset of action
than sumatriptan; frovatriptan (Frova), naratriptan (Amerge), and eletriptan
have longer half-lives than sumatriptan. In practice, route of administration
or pharmacokinetics often guide choice. Some triptans are available as nasal
sprays, rapidly dissolving tablets (absorbed despite vomiting), or subcutaneous
injections. Some physicians choose a triptan by matching pharmacokinetics to
the temporal pattern of their patient’s migraine (e.g., rapidonset medication
for short course of migraine versus longer-acting medication with slower onset
for longer lasting symptoms); however, there is no definitive evidence to
support this approach. The vasoconstrictive properties of triptans preclude
their use in patients with ischemic heart disease, stroke, uncontrolled
hypertension, or hemiplegic or basilar migraine. However, the chest pain
occurring in 3 to 5 percent of oral triptan users has not been associated with
electrocardiographic changes and is rarely ischemic. A post-marketing study of
subcutaneous sumatriptan in 12,339 patients without ischemic heart disease
revealed 36 cardiac events, only two of which occurred within 24 hours of
sumatriptan use (O’Quinn S, Davis RL,
Gutterman DL, Pait GD, Fox AW. Prospective largescale study of the tolerability
of subcutaneous sumatriptan injection for acute treatment of migraine.
Cephalalgia. 1999;19(4):223-231). Nonetheless, if patients taking triptans
develop suspected cardiac symptoms, triptans should be discontinued pending
further evaluation. Cardiac evaluation is reasonable before triptan initiation
in patients with multiple vascular risk factors.28 Triptans are contraindicated
in patients taking monoamine oxidase inhibitors. Combining triptans with
selective serotonin reuptake inhibitors can lead to serotonin syndrome, a
potentially life-threatening condition characterized by altered mentation,
autonomic instability, diarrhea, neuromuscular hyperactivity, and fever. The
true incidence of serotonin syndrome in this setting is unknown. A 2006 U.S.
Food and Drug Administration (FDA) alert cited 29 case reports over five years,
although almost 700,000 patients per year are prescribed both selective
serotonin reuptake inhibitors and triptans (Sclar
DA, Robison LM, Skaer TL. Concomitant triptan and SSRI or SNRI use: a risk for
serotonin syndrome. Headache. 2008;48(1):126-129). Physicians treating
patients who are taking triptans and selective serotonin reuptake inhibitors
should be vigilant for serotonin syndrome, and should minimize drug dosages.
NSAIDs are
a convenient first-line therapy for mild to moderate migraine or historically
responsive severe attacks. A 2007 meta-analysis of ibuprofen for moderate to
severe migraine showed that 200-mg and 400-mg doses were effective for
short-term pain relief, but had 24-hour pain-free rates similar to placebo. The
400-mg dose also helped relieve photophobia and phonophobia. A study comparing
ketoprofen with zolmitriptan showed zolmitriptan to be modestly more effective
(two-hour relief in 61.6% versus 66.8% of participants, respectively), but it
was associated with more adverse events, such as tight throat and flushing (Dib M, Massiou H, Weber M, Henry P,
Garcia-Acosta S, Bousser MG; Bi-Profenid Migraine Study Group. Efficacy of oral
ketoprofen in acute migraine: a double-blind randomized clinical trial.
Neurology. 2002; 58(11):1660-1665). Ketorolac, a parenteral NSAID commonly
used in emergency departments, was found to be effective in reducing
selfreported headache symptoms one hour after injection, including one study
showing more effectiveness than intranasal sumatriptan.
Description of cases
Case 1: LR is a 57 manager in a multinational company and his
job includes many trip, both by car and plane, to visit customer all over Italy
and to visit the Headquarters in Northern Europe. He initially presented the
first symptoms of a left sided migraine in September 2013. It appeared suddenly
without previous symptoms or neck stiffness. It was initially treated by his GP
with Ibuprofen (200 to 800 mg orally every 6 to 8 hours, not to exceed 2.4 g
per day) and, later, with Naproxen (250 to 500 mg orally every 12 hours, not to
exceed 1 g per day) but the therapy did not work out and the patient started
suffering heartburn, gastric rebound headache, and his renal function
degenerated (Creatinine was 0.95 in Sept 2013; 1.3 in Mar 2014 and 1.9 in Oct
2014) so he decided to ask a neurologist who suspended the therapy with NSADIs
and introduced Sumatriptan (oral: 25 to 100 mg, can be repeated in 2 hours, not
to exceed 200 mg per day) which only controlled the symptoms. He arrived at our
observation on request of the neurologist in Feb 2015 to evaluate any possible
psychiatric and psychosomatic involvement.
Case 2: AR is an unemployed 35-year-old guy. He came into
observation in Nov 2014 for a right-sided headache with aura resistant to
classical NSADIs and cortisone. He was initially treated with Zolmitriptan
(oral disintegrating tablets: 2.5 mg, can be repeated in 2 hours, not to exceed
10 mg per day) with weak results.
Treatment: both cases were initially treated with osteopathic
manipulation and with re-educational posture exercises. During the treatment
drugs were systematically reassessed and decreased. After 24 weeks of treatment
(in Aug 2015), LR had been symptoms-free for 10 days and drugs were definitely
suspended. During the December’s follow up he reported he had no more symptoms
since then. After 16 weeks of treatment (in Mar 2015), AR stopped taking any
drug and kept only the posture treatment for 3 more weeks. After this period he
had no more symptoms.
Discussion
The most
important factor in a true migraine syndrome is the position of the C1 and C2
vertebrae, the top two vertebrae in the neck. These two structures are
completely unique in comparison to the rest of the vertebrae. The ellipsoidal
joints between the occipital bone (the base of the cranium) and C1 and the
similar joint between C1 and C2, allow for a great deal of mobility at this
level of the spine. This high degree of mobility here opens up the possibility
for some negative effects on the vertebral artery and veins, as well as the
brainstem itself, when these structures move into a distorted position. Where
blood flow to and from the cranium is provided by the vertebral arteries and
veins is concerned, opposing rotations of the C1 and C2 seem to have the
biggest influence on migraine headache. When one of these structures is rotated
to the right while the other is rotated to the left a great deal of compression
of these vascular structures occurs. Since veins are much easier to compress
than arteries, blood flows more easily into the intracranial space, the area
around your brain, than out of it. Blood then becomes trapped inside the
cranium increasing the pressure there, triggering migraine headache pain.
Medical theories relating to the vasodilation causes by certain neuropeptides
is a cause of migraine headache. One explanation for the presence of these
neuropeptides could be that the body is trying to deal with increased blood
pressure in the head that occurs as described above. In examining the cadavers
of migraine sufferers, this opposing rotation of C1 and C2 has been observed by
our staff in conjunction with patterns of the cranial vascular system that have
been imprinted on the internal bony surface of the cranium due to the high
degree of pressure in those structures. Eliminating these distortions of C1 and
C2 is been vital in eliminating migraine headache in our patients.
There are
other implications for the nervous system when C1 and C2 are distorted. At this
level the brainstem is extending down into the spinal canal before
transitioning to the spinal cord at about C3. A cranial nerve emanating from
the brainstem, the trigeminal nerve has been implicated as a source of migraine
headache. The trigeminal nerve is an extremely sensitive nerve that is
responsible for sensation and function in the jaw, teeth, face, tongue, lips,
eyes, sinuses and the brain itself. When C1 and C2 become distorted, a
reduction in the space that the brainstem occupies occurs. This intrusion into
the brainstem can especially be seen when the C1 projects or shears forward on
the C2. In this case part of the C2, called the odontoid process, can begin to
migrate backwards, compressing the brainstem and cranial nerves, including the
trigeminal nerve. When this process begins, disruption of many neurological
functions can occur contributing to migraine pain that stems from these
structures. Once again, we see postural distortion jeopardizing a critical area
of the body.
Conclusions
The role of
postural distortion in conditions such as hip or back pain is obvious. When we
recognize that these distortions have a profound effect on vital structures in
the cervical spine and cranium, we have a tremendous opportunity to create
healing. It might seem strange that, in order to eliminate migraines, we might
have to treat muscles in your thighs. However, along with very specific
structures in the neck and head, it is, so, important to look at all facets of
postural distortion in order to alleviate pain. As with our approach to
relieving pain in any situation, creating balance and symmetry is the key.
Authors: T. Candiani, A. Aceranti, A. Simone, M. Tuvinelli, S. Vernocchi
Published: Italian Journal of Medicine, vol 10, suppl 2, May 2016
Presented: Poster FDI6738-27at the FADOI National Congress of Medicine, 2016
Download the full article:
https://aceranti.it/wp-content/uploads/2022/01/Treatment-of-unilateral-migraine-with-triptans-versus-posture.pdf
(se il link non funziona fai copia-incolla nel tuo browser)