Vertebral spondylodiscites or osteomyelitis are infectious processes of
the spinal column. This type of infection can affect the vertebrae in isolation
(spondylitis), the discs (discitis) or both (spondylodiscitis).
Background and purpose of the study: The incidence presents a first, prevalent peak in adults after the age of 50 and a second, lower peak, during the second decade of life, from 10 to 20 years. In children, the rich vascularization of the immature disc favors the onset of discitis (3% of cases, without sex difference). The vascularity of the disc disappears at the age of 20 and therefore in adults the infection develops primarily in the vertebra, extending only secondarily to the disc, configuring the typical picture of spondylodiscitis. The anatomical structures contiguous to the vertebral column, from the meninges, to the medulla, to the nerves and to the paravertebral muscles can also be involved in varying degrees by the infectious process. The infectious process can be localized at all levels of the spinal column, most frequently in the lumbar tract (60-70% of cases).
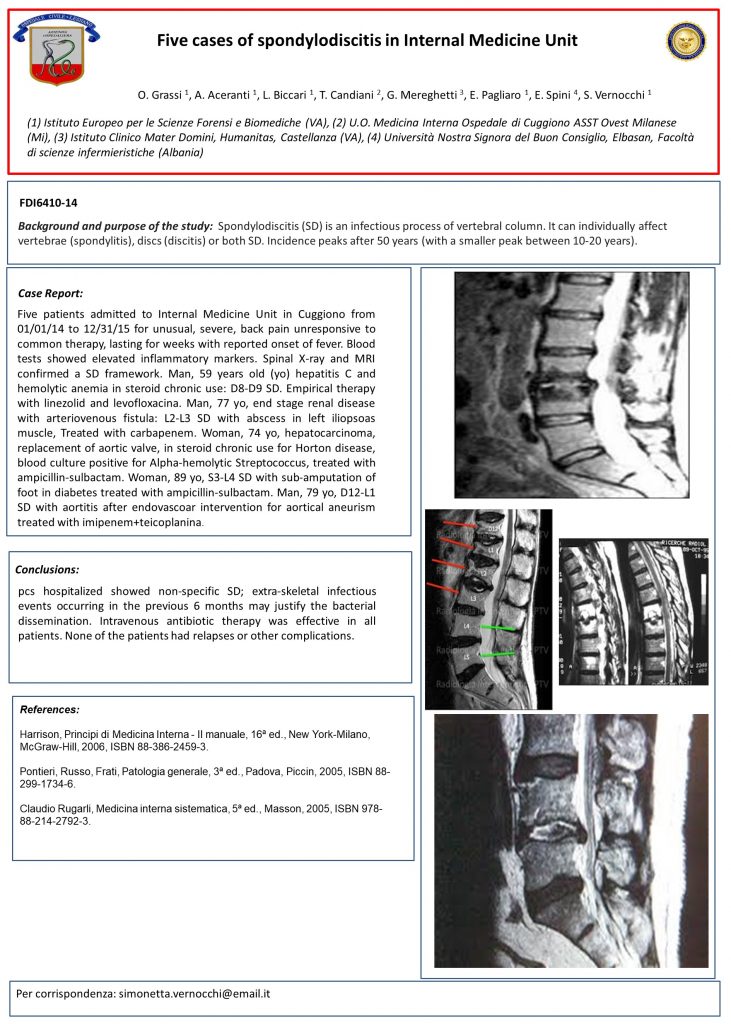
Description of the cases: Five patients admitted to Internal Medicine Unit in Cuggiono from 01/01/14 to 12/31/15 for unusual, severe, back pain unresponsive to common therapy, lasting for weeks with reported onset of fever. Blood tests showed elevated inflammatory markers. Spinal X-ray and MRI confirmed a SD framework. Man, 59 years old (yo) hepatitis C and hemolytic anemia in steroid chronic use: D8-D9 SD. Empirical therapy with linezolid and levofloxacina. Man, 77 yo, end stage renal disease with arteriovenous fistula: L2-L3 SD with abscess in left iliopsoas muscle, Treated with carbapenem. Woman, 74 yo, hepatocarcinoma, replacement of aortic valve, in steroid chronic use for Horton disease, blood culture positive for Alpha-hemolytic Streptococcus, treated with ampicillin-sulbactam. Woman, 89 yo, S3-L4 SD with sub-amputation of foot in diabetes treated with ampicillin-sulbactam. Man, 79 yo, D12-L1 SD with aortitis after endovascoar intervention for aortical aneurism treated with imipenem+teicoplanina.
Conclusions: pcs hospitalized showed non-specific SD; extra-skeletal infectious events occurring in the previous 6 months may justify the bacterial dissemination. Intravenous antibiotic therapy was effective in all patients. None of the patients had relapses or other complications.
Authors: O. Grassi, A. Aceranti, L. Biccari, T. Candiani, G. Mereghetti, E. Pagliaro, E. Spini, S. Vernocchi
Published: Italian Journal of Medicine 2016
Presented: Poster FDI6410-14 at the FADOI National Congress of Medicine 2016